Melanoma
The incidence of melanoma has been on the rise for decades, maybe due to damage to the ozone layer in atmosphere. Presently, it is the seventh common cancer in the United States. The estimated lifetime risk of developing skin melanoma in Americans was 1 in 1,500 in 1935 and is expected to rise to 1 in 75 by year 2000. Melanoma can affect individuals in their 20's and 30's but the average age at the time of diagnosis is between 55 and 57. This cancer starts in the skin. The most frequent sites in women are the arms and legs, and in men it is the trunk. It is more common in fair-skinned individuals and significantly less common in African-Americans and individuals with dark color skin.
Cause
Heavy exposure to sun is the most important factor in development of melanoma. It is more common in individuals who develop sunburn or blister from excessive exposure. Certain skin moles can also transform into melanoma.
Signs and Symptoms
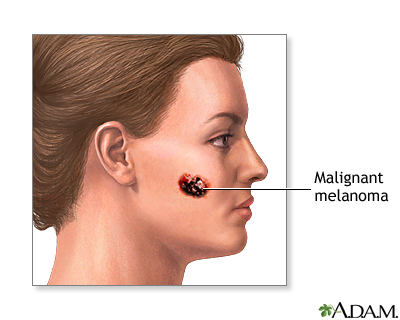
Patients do not have any signs at very early stages. Most commonly, a mole is noticed to be getting bigger rapidly, or bleeding. Larger moles with irregular shapes and borders, a deep black color, may represent a melanoma. Such moles must be removed and examined. On occasion, the disease may have spread to other organs and may present with signs of advanced disease: cough, shortness of breath, chest pain or blood in the sputum are among early worrisome signs. Other signs of this illness could be weakness, fatigue, weight loss and bone pain.
Establishing Diagnosis
When the diagnosis is suspected, patients have to be examined carefully by a qualified physician. Diagnosis in a patient who has a cancerous mole is made by removal and analysis of the mole. In certain patients, the cancer may have already spread to lymph glands in the neck, under the arms, or in the groin area. In such cases, fine needle aspiration of the node should be performed, which may lead to the diagnosis of this illness.
Staging
The prognosis of melanoma is directly related to the extent and depth of skin penetration at diagnosis. Clark's method is a microscopic evaluation of the site of the original melanoma mole. There five stages to this system, Clark 1 being the most superficial and 5 being the deepest invasion of the skin and penetration into fatty tissue under the skin. Sentinel Node biopsy is a newer method of evaluating lymph node involvement.
Treatment
The only effective treatment for this disease is a successful surgical removal of the involved skin. A suspicious lesion is normally removed to establish the diagnosis. If the diagnosis is of a Melanoma, then a second surgery of a wider area of normal skin around the original site must be performed. Curative surgery is incomplete without this wide excision. The role of more aggressive surgery, removing the local lymph glands, is very vague and unclear.
Although one can remove the mole with surgery, however cancer cells may have already spread to other parts of the body. Detection of these cells at these early stages and with our current knowledge and technology is not possible. Clinical trials have shown that adjuvant therapy with Interferon following surgery on high-risk melanomas will reduce the recurrence rate and will prolong survival of patients. Interferon remains the most active adjuvant therapy for Melanoma.
When the disease spreads to other site, i.e. metastatic stage, it becomes a difficult challenge to treat. Most treatment regimens use a combination of various chemotherapy drugs along with Immunotherapy with Interferon, Interleukin 2 or Melanoma Vaccine.
A rather aggressive and established regimen that is used frequently in metastatic melanoma is referred to Dartmouth Regimen and consists of:
- BCNU given every six weeks
- DTIC given daily for three days, every three weeks.
- Cisplatinum given daily for three days, every three weeks.
- Tamoxifen twice daily
Other drugs that may be used are Vinblastine, Bleomycin which may induce a minimal response in some patients.
The one treatment that seems to be more effective is Interleukin 2. This drug has been used in a variety of schedules and doses with almost 20% response rate, however 5-6% of patients have achieved very durable responses lasting over 5 years. Among patients who achieve a complete response to Interleukin 2, almost 80% become long term survivors with no recurrence of melanoma.
Staging workup for metastatic melanoma
Once a diagnosis of the metastatic melanoma is established, a thorough examination of the patient should be done to disclose crucial information. CT scan of chest and abdomen and a bone scan should be performed to determine the extent of the spread. Additional tests include CT scan of the brain and a bone marrow test. The purpose of these tests is to look in the tissues and organs where cancer has a tendency to spread.
Patterns of spread
Melanoma can spread locally and involve nearby tissues, such as the local lymph glands or liver, bones, brain or lungs. Another organ where melanoma tends to spread to are the Adrenal glands, which are the glands located above the kidneys and which produce special hormones. Cancer can also spread to the area near spinal cord and vertebrae.
Special Situations
Patients with advanced melanoma may develop any of the following complications.
- Pleural effusion
- Pericardial effusion
- Spinal cord compression
- Brain metastasis
- Bone metastasis
- Paraneoplastic syndromes
- High Calcium level
- Pain
Survival and Prognosis
Survival of patients with metastatic melanoma will depend on the type and extent of the cancer at the time of initial diagnosis. Prognosis depends primarily on the depth of skin involvement and thickness of the tumor. Some patients with early stages of melanoma of the skin may be cured with surgery alone. With patients in whom cure is not possible survival could vary from months to years, depending on the extent of cancer, overall condition of the patient, his/her response to treatments and the duration of that response.
Follow-up
After completion of treatment in any combination that might have taken place, patients need to remain under surveillance for the possibility of a recurrence of melanoma. Follow-up should be scheduled on a regular basis, initially every one to three months for one to two years, and thereafter less frequently. A thorough skin examination by a skin specialist (Dermatologist) has to be done at least once a year. Patients must avoid excessive sun exposure. The frequency of follow-up will depend on the condition of the patient and his/her disease. In each follow-up visit, a patient is examined and, normally, a chest x-ray is obtained every few months. A CT scan of the chest and a bone scan are done once a year.
Treatment of recurrent disease will depend on the stage and extent of the reoccurred disease. These patients are treated with chemotherapy utilizing the same agents as mentioned above. Radiation therapy may be helpful in managing painful or symptomatic areas, where the cancer has spread. For patients who experience pain, various pain medications may be used to alleviate pain. For patients with advanced disease, where most treatments have failed, one could consider assistance from Hospice.
Melanoma
Melanoma
Melanoma
Melanoma
Melanoma
Melanoma
Melanoma